Warum ist die UV-Lichttherapie so wichtig für die Gesundheit unserer Haut?
What is Ultraviolet light?
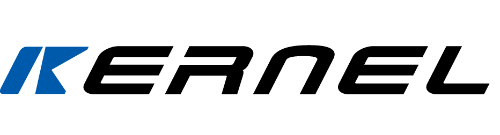
Ultraviolet light refers to the electromagnetic spectrum with wavelengths in the range of 180-440nm, which is divided into ultraviolet A, UVA, ultraviolet B, UVB and ultraviolet C.
Wavelength of ultraviolet light
UVA: wavelength 320-400nm, Strong penetration ability
UVB: wavelength 280-320nm, medium Penetration ability
UVC: wavelength 180-280nm, weak penetration ability
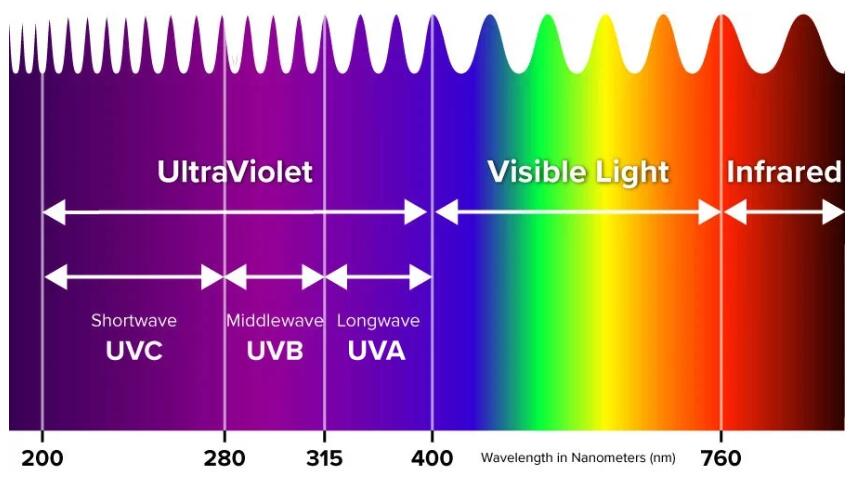
UV light in sunshine
Ultraviolet rays in sunlight also include UVA, UVB and UVC.
The intensity of sunlight's ultraviolet rays is affected by latitude, altitude, clouds, atmosphere and other particles. In our living environment, UVA accounts for 90%-95%, UVB accounts for 5%-10%, and UVC is almost entirely absorbed by the ozone layer.
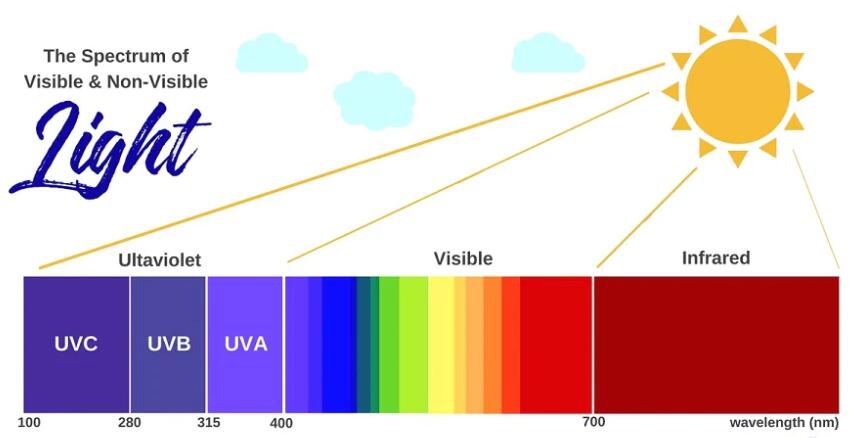
The depth of UVA and UVB reaching the skin surface can reach the dermis and epidermis respectively.
An individual's dose of UV rays from the sun depends on the time spent outdoors and the use of UV-protective clothing and sunscreen.
Artificial UV light
For the needs of medical diagnosis and treatment, scientists invented ultraviolet lamps to emit ultraviolet light in a specific waveband with controllable power and energy. General ultraviolet treatment in dermatology is optical treatment based on artificial ultraviolet light.
The main physiological effects of ultraviolet rays on skin
Penetration depth of ultraviolet rays into the skin
UVA can penetrate into the superficial layers of the dermis and subcutaneous tissue
Most of the UVB is absorbed by the epidermis, and a small amount reaches the dermis.
Almost all UVC (artificial ultraviolet rays) are absorbed by the epidermis
Pathophysiological effects of ultraviolet rays on skin
Ultraviolet rays can upregulate melanin production and promote the accumulation of melanin in the epidermis
Ultraviolet rays can promote the division of epidermal keratinocytes, leading to an increase in epidermal thickness
UV rays can cause immune tolerance or immunosuppression
Ultraviolet rays can promote the conversion of 7-dehydrocholesterol into vitamin D3, thereby producing vitamin D
UV rays induce a cascade of release of vasoactive and neuroactive mediators in the skin, leading to an inflammatory response
High-intensity ultraviolet light exceeds the threshold damage response and can directly induce keratinocyte apoptosis
UVA can produce reactive oxygen (ROS) and indirectly damage cellular DNA
Categories of UV Light therapy
Ultraviolet therapy is a physical method that uses ultraviolet rays of a certain wavelength to treat skin diseases under the guidance of a certain light dose, exposure time and treatment plan.
Currently, ultraviolet treatments commonly used in clinical dermatology include:
Narrow band uvb(NB-UVB,311nm) treatment
UVB ( BB-UVB,280-32nm) light therapy
308nm excimer( laser) treatment
UVA1 (340-400nm) treatment
PUVA treatment
Ultraviolet A and B(280-400nm) treatment
UV light treatment mechanism
Immunosuppressive
Induces apoptosis or necrosis of Langerhans cells and downregulates the number of epidermal Langerhans cells
Reduced Langerhans cell antigen uptake, processing, presentation and migration capabilities
Downregulates expression of intercellular adhesion molecules in Langerhans cells
Induces skin T cell apoptosis
Convert trans-urocanic acid in the epidermis into cis-urocanic acid, thereby suppressing immunity by inhibiting neutrophil activity and other pathways
It is the main mechanism for treating skin diseases such as psoriasis, vitiligo, and cutaneous T-cell lymphoma.
Anti-inflammatory and anti-allergic
Induces mast cell apoptosis, inhibits mast cell degranulation and histamine release
Inhibition of T cell-induced delayed hypersensitivity reactions (treatment of contact dermatitis)
Upregulates interleukin IL-1 receptor antagonist to regulate excessive inflammatory response
It is the main mechanism for treating inflammatory, allergic and itchy skin diseases.
Promote melanin production
Increases melanin production and promotes melanin accumulation in the epidermis
The most obvious UV is around 300-400nm band
It is the main mechanism for treating hypopigmentation or depigmentation skin diseases such as vitiligo.
Antiproliferative effect
Anti-angiogenesis
Enhance skin UV tolerance
Anti collagen proliferation
Features of kinds of UV light therapy
NB-UVB phototherapy
It is the most commonly used ultraviolet treatment method at present.
In most cases, more effective than BB-UVB
Few adverse reactions, less erythema and blisters
For vitiligo, psoriasis, atopic dermatitis, polymorphic light eruption, eosinophilic pustular folliculitis, parapsoriasis, mycosis fungoides, chronic urticaria, localized scleroderma, lichen planus, rosea The curative effect is remarkable on diseases such as pityriasis, chronic lichenoid pityriasis, and lymphomatoid papules.
NB-UVB has no significant correlation with the occurrence of skin cancer and has good long-term safety
BB-UVB phototherapy
An earlier method of ultraviolet treatment
Before the emergence of NB-UVB, BB-UVB was mainly used for the treatment of parapsoriasis
Currently, it has unique advantages in the treatment of skin pruritus and parapsoriasis (chronic pityriasis lichenoidosa, acute acne-like pityriasis licheniformis)
308nm excimer (laser) light therapy
Suitable for the treatment of localized psoriasis vulgaris and vitiligo
Good targeting, good efficacy, short treatment course, and few adverse reactions
Disadvantages: small light spot, high treatment cost
Penetrates deep into the reticular layer of the dermis
Can act on fibroblasts, dendritic cells and inflammatory cells deep in the skin, such as T lymphocytes, mast cells and granulocytes
UVA1 treatment is divided into low dose (10-20J/cm2), medium dose (20-70J/cm2) and (70-130J/cm2)
Filters out the UVA2 band that is prone to erythema, without the phototoxic side effects of psoralen treated with PUVA
PUVA treatment
Oral administration of 8-methoxypsoralen (8-MOP) and 5-methoxypsoralen (5-MOP) before treatment to enhance UV efficacy
It has good effects on vitiligo, palmoplantar pustulosis, plaque parapsoriasis, cutaneous T-cell lymphoma, lymphomatoid papulosis, lichen planus, and mastocytosis.
Psoralen is phototoxic and requires sun protection after PUVA treatment.
Oral route of administration may cause intestinal opacity reaction
UVAB phototherapy
Combined treatment of UVA and BB-UVB.
The treatment of atopic dermatitis is more effective than UVA or BB-UVB alone
Poor effectiveness and safety, currently not commonly used